
A crisis intervention team (CIT) is a police mental health collaborative program found in many American cities. The term “CIT” is often used to describe both a program and training in law enforcement that helps guide interactions between law enforcement and those living with mental illness.
The purpose of a CIT program is to safely assist individuals living with behavioral health issues or who are experiencing behavioral health crises, including mental illness, a mental disability or substance use disorders, by connecting them with available services through comprehensive collaboration among law enforcement and the community and through specialized responses and training.
There are many benefits for developing a police department crisis intervention program. Benefits include reduced arrests of people with mental illness and improved officers’ attitudes and knowledge about mental illness. There is also an increased likelihood that individuals will receive mental health services, and police officers will be provided with more tools to do their jobs safely and effectively.
MCT members undergo specialized training to equip them with the necessary skills for crisis intervention and support.
The primary goals of CIT are to reduce injuries to officers and mental health consumers during contact and to appropriately redirect mental health consumers from the judicial system to the services and support needed to stabilize these individuals and reduce contact with police. As early intervention services are provided, the team can assess and refer to a variety of community programs, including emergency assistance, psychiatric services, therapy, housing and outreach. Additional programs can provide substance use and recovery and comprehensive community support services.
Training is a critical aspect of a successful CIT program. Mental health-related classes are taught by crisis intervention coordinators, a team of four detectives with expertise in specialized areas.
The Albuquerque, New Mexico, Police Department has implemented a broad-based CIT training program. These include the following components:
- Cadets basic academy training: Consists of a 40-hour basic CIT class.
- CIT-certified field officers: These officers receive a 40-hour advanced course. They are baseline-trained mental health responders. They are generalists who take mental health calls when no specialized response is available. 100% of non-probationary field officers and nearly 100% of sergeants have been trained. Specialized unit detectives are included in this group.
- Enhanced CIT or ECIT officer training: Consists of a voluntary advanced class. Around 50% of the field is certified as ECIT. Training consists of an eight-hour class with a refresher class every two years. Training is focused on advanced topics in behavioral health, including suicide intervention strategies. ECIT officers are trained to prepare certificates for mandatory evaluations. They are the backbone of APD’s field mental health response, with over 200 uniformed officers, including several in each area command on each shift. These officers respond to the highest-risk mental health calls, such as armed individuals and individuals threatening suicide from an elevated platform.
- Telecommunicators training: Consists of 20 hours of training for 9-1-1 call-takers and police dispatchers. Their training includes mental health first aid and scenarios based on actual received crisis calls.
- Police service aides training: Requires 16 hours, including mental health first aid and scenario-based training.
- Mobile crisis teams (MCT): A collaboration between the City of Albuquerque and Bernalillo County, which responds to individuals experiencing a nonviolent behavioral health crisis that necessitates a 9-1-1 response. New Mexico has implemented mobile crisis intervention teams with approval from the U.S. Department of Health and Human Services (HHS). These teams connect eligible individuals in crisis to behavioral health providers 24/7, 365 days a year. Four APD teams and two Bernalillo County Sheriff’s Office teams are available from 10 a.m. to 11 p.m.

The MCT initiative aims to provide rapid response, individual assessment, stabilization and de-escalation to people with Medicaid who need immediate support. The six MCTs provide specialized responses to 9-1-1 calls involving a behavioral health element. These are primarily nonviolent calls combined with “gray-area calls.”
This is a co-responder model: two-person response teams with an ECIT-trained law enforcement member and an MCT-trained master’s-level behavioral health clinician. MCT clinicians are independently licensed mental health professionals who work in a team with a uniformed law enforcement officer. Clinicians can write certificates for evaluation and safety plans.
MCTs co-respond to high-level mental and behavioral health emergencies. MCT clinicians provide professional behavioral health services to de-escalate crises and link individuals who are experiencing mental health emergencies to appropriate services in the community.
Currently, MCTs only respond to calls in the 9-1-1 system. When someone in crisis calls 9-1-1, the dispatcher will ask questions to determine if they are appropriate for an MCT response. MCTs can also be requested by field officers who are on the scene of a call. Services provided by MCTs include:
- Assessment: MCTs assess the individual’s situation and needs.
- Crisis intervention: They provide immediate support and de-escalation.
- Supportive counseling: MCTs offer counseling to help individuals cope with their crises.
- Information and referrals: They connect people to community-based mental health services.
- Transport to Psychiatric Emergency Room: If necessary, MCTs arrange transportation to a hospital psychiatric emergency room.
MCT members undergo specialized training to equip them with the necessary skills for crisis intervention and support. There are several key aspects of their training. Assessment and safety evaluation is an important topic. MCT members assess the severity of the crisis and the individual’s immediate risk. They ask about suicidal thoughts, plans and intent. If the person is actively suicidal, MCT members prioritize safety by ensuring the removal of any lethal means (e.g., weapons, medications).
Active listening and empathy are skills required for MCTs. MCTs listen attentively and empathetically to people’s feelings and experiences. They validate the person’s emotions and express understanding without judgment.
MCT members work collaboratively with the individual to create a safety plan. The safety plan includes coping strategies, emergency contacts, and steps to take during a crisis. They identify supportive people in the person’s life who can be contacted during difficult moments.
MCTs will discuss engagement with support systems by encouraging the person to reach out to friends, family or mental health professionals. They provide information about crisis hotlines and local resources. Depending on the level of risk, MCT members may recommend a referral for hospitalization or other intensive services. If immediate hospitalization is necessary, they arrange for transportation to a psychiatric emergency room.
MCTs follow up with the individual after the crisis to ensure their well-being. They provide information about ongoing mental health services and encourage the person to seek professional help. MCT members are trained to handle these situations with compassion and expertise. When MCT members encounter individuals in suicidal crises, they follow a structured approach to provide immediate support and safety.
Post-crisis: Crisis intervention unit (CIU)
APD has implemented a post-crisis intervention unit in the program. They contract with a medical director from a local hospital and have a department-employed psychiatrist who heads the Behavioral Health Division. These individuals oversee the civilian CIU clinicians who assist home visit detectives by conducting risk assessments, writing certificates for evaluation and providing safety plans. These are all licensed master’s-level clinicians with Clinical Mental Health Counselor certifications.
The CIU home visit detectives attempt to divert individuals from the 9-1-1 system to community services. They follow up on higher-risk cases with a history of violence and/or suicide attempts with weapons. These detectives are experts in resource knowledge, provider contacts and diversion through community services. The CIU complements both the ECIT and MCT programs.
In summary, CIT programs and specialized mobile crisis teams play a vital role in providing timely and effective support during behavioral health crises. The existing research suggests a CIT program and the mobile crisis team model are promising approaches to reduce unnecessary emergency departments and hospital admissions and connect individuals to needed services. Generally, the limited research on stakeholder perceptions suggests that providers, police officers and consumers (i.e., patients and their family members) view the team positively and have high rates of overall satisfaction.
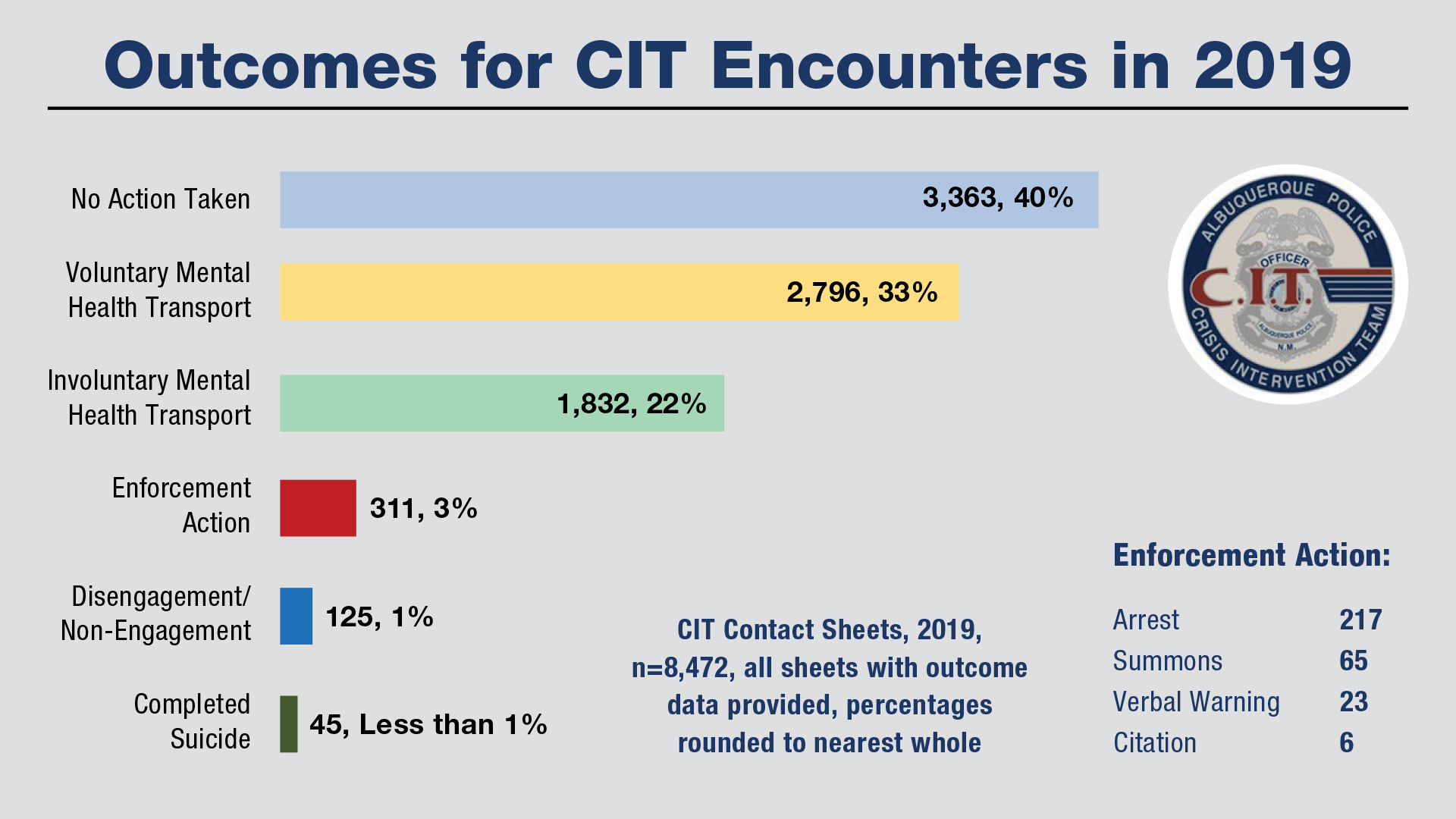
The chart above depicts the outcome of all CIT encounters in 2019 for the Albuquerque Police Department. Data like this is critical to evaluating the impact of an agency’s program. In addition to this data, APD found that uses of force in these matters were significantly reduced from previous years. With significant variations across models in terms of programmatic elements (e.g., staffing, availability), populations served and main referral sources, it is challenging to draw broad conclusions across studies in terms of the model’s effectiveness. Additional research regarding their effectiveness and impact is needed. From a community perspective, however, effective CIT programs will increase legitimacy and trust in a police department.
As seen in the August 2024 issue of American Police Beat magazine.
Don’t miss out on another issue today! Click below:





